In the realm of maxillofacial reconstruction, a significant breakthrough has emerged from the labs of the Military Institute of Engineering in Rio de Janeiro, Brazil. Researchers, led by Marvin do Nascimento from the Department of Materials Engineering, have developed a novel approach to enhance the bioactivity of Polymethylmethacrylate (PMMA) prostheses, potentially revolutionizing facial bone reconstruction.
The study, published in ‘Academia Materials Science’ (translated to English as ‘Academic Materials Science’), focuses on coating PMMA prostheses with hydroxyapatite (HA), a mineral naturally found in human bones. This innovation aims to address the limitations of PMMA’s bioinert nature, which often results in poor tissue integration.
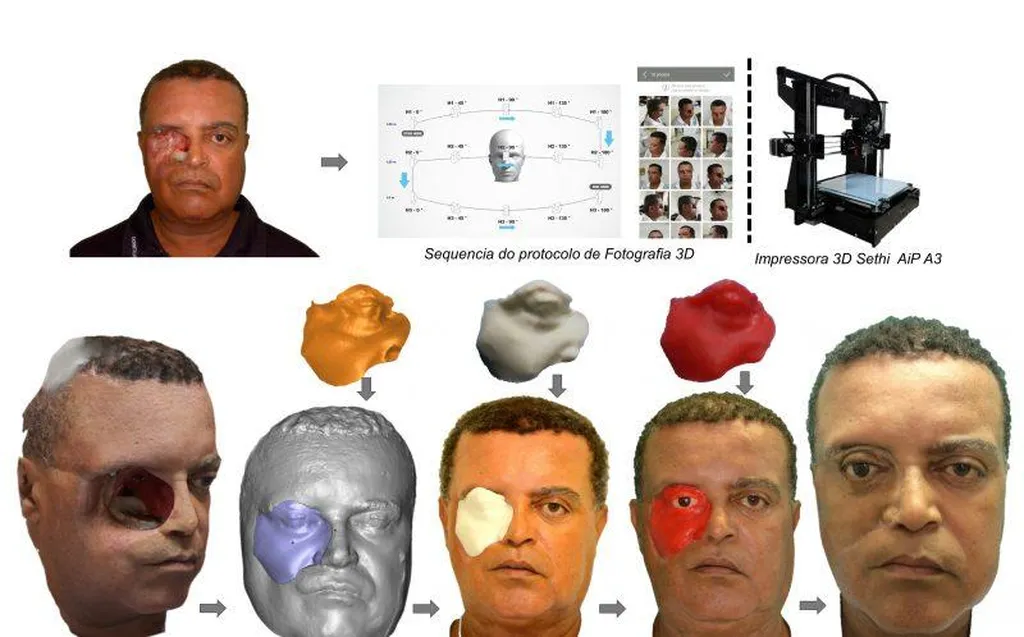
Do Nascimento and his team fabricated two prototypes using additive manufacturing, each with distinct porous configurations. Prototype A featured ellipsoidal pores, while Prototype B showcased a regular hexagonal architecture. Both designs underwent rigorous mechanical evaluations, demonstrating impressive tensile strength, impact toughness, and flexural strength, ensuring structural stability under functional demands.
“The integration of controlled porous architecture with HA deposition resulted in composite prostheses that combined mechanical robustness with surface bioactivity,” said Do Nascimento. This combination is crucial for improving the interaction between the prosthesis and biological tissues, ultimately enhancing the outcomes of maxillofacial reconstruction.
Structural analysis revealed the formation of calcium phosphate phases with low crystallinity, predominantly hydroxyapatite and octacalcium phosphate. Surface examination showed a continuous granular coating with pseudo-spherical agglomerates, indicating successful HA deposition.
Bioactivity assays further highlighted the potential of HA-coated prostheses. While uncoated PMMA remained bioinert, the coated versions were capable of inducing apatite precipitation, a key factor in promoting tissue integration.
Prototype A favored permeability and surface area for potential cell adhesion, while Prototype B ensured uniform porosity and predictable load distribution. These findings suggest that the choice of porous architecture can be tailored to specific clinical needs, offering a more personalized approach to maxillofacial reconstruction.
The commercial implications of this research are substantial. Enhanced bioactivity and improved tissue integration can lead to better patient outcomes, reduced need for revision surgeries, and ultimately, lower healthcare costs. Moreover, the use of additive manufacturing allows for the production of customized prostheses, catering to the unique anatomical requirements of each patient.
This study represents a promising step forward in the field of maxillofacial reconstruction. As Do Nascimento noted, “The results open new avenues for the development of advanced biomaterials that can mimic the complex structure and function of natural bone.”
The research not only highlights the potential of HA-coated PMMA prostheses but also underscores the importance of interdisciplinary collaboration in driving innovation. By combining materials science, engineering, and medical expertise, this study paves the way for future developments in the field of maxillofacial reconstruction and beyond.