In a groundbreaking development that could revolutionize the treatment of tumor-derived osteochondral defects (OCDs), researchers have introduced a novel microneedle platform that combines precise tumor ablation with coordinated cartilage and bone regeneration. This innovative approach, detailed in a study published in *Bioactive Materials* (which translates to *Active Biological Materials* in English), offers a minimally invasive solution for a complex clinical challenge.
The research, led by Jinpeng Wang from the Center for Orthopedic Science and Translational Medicine at Shanghai Tenth People’s Hospital and Tongji University, along with the Yantai Key Laboratory for Repair and Reconstruction of Bone and Joint, presents a spatiotemporal microneedle (MN) platform. This platform synergistically combines protoporphyrin IX (PpIX)-mediated sonodynamic therapy (SDT) for targeted tumor eradication with chondral organoid (CO)-driven regeneration.
“Our goal was to create a system that not only eliminates tumors but also promotes the regeneration of cartilage and bone in a coordinated manner,” said Wang. “By leveraging differential mechanical cues, we can guide the lineage-specific development of chondral organoids, ensuring effective and targeted healing.”
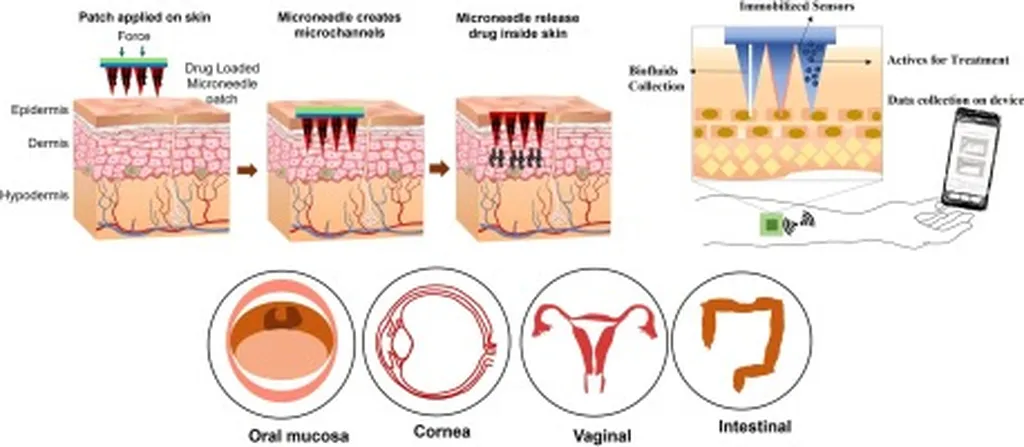
The study highlights the engineering of COs from bone marrow stem cells (BMSCs) using agarose microwells. These COs matured into hyaline-like phenotypes over 30 days and demonstrated superior resilience to oxidative stress compared to monolayer BMSCs. The microneedles were fabricated from gelatin methacryloyl (GelMA) in a bilayer architecture, with stiff tips to facilitate penetration and promote osteogenesis, and a softer base to enhance chondrogenesis. PpIX and COs were co-encapsulated for targeted delivery.
In vitro studies showed that MN(+PpIX) under ultrasound induced robust ROS generation, apoptosis, and proliferation inhibition in giant cell tumor of bone (GCTB) cells via NF-κB modulation. In vivo, in a subcutaneous GCTB xenograft model, MN-mediated SDT significantly reduced tumor volume and enhanced apoptosis. In a rabbit knee OCD model, MN(+PpIX/CO) achieved superior integrated osteochondral repair, with improved bone volume fraction, trabecular thickness, and higher O’Driscoll/ICRS scores compared to controls.
The implications of this research are profound. “This platform innovatively sequences SDT and regeneration, using stiffness gradients to guide CO fate,” Wang explained. “It offers a minimally invasive solution for tumor-associated OCDs, potentially transforming the way we approach these complex clinical challenges.”
The study’s findings could pave the way for new treatments that not only address the immediate threat of tumors but also promote long-term healing and regeneration. As the field of regenerative medicine continues to evolve, this research provides a compelling example of how innovative technologies can be harnessed to improve patient outcomes and shape the future of medical treatments.
With the publication of this research in *Bioactive Materials*, the scientific community now has a robust framework to build upon, potentially leading to breakthroughs in the treatment of osteochondral defects and other related conditions. The commercial impacts for the medical and biotechnology sectors are substantial, offering new avenues for product development and therapeutic interventions.