In a groundbreaking development poised to revolutionize bone regeneration, researchers have unveiled a novel 3D-printed scaffold that promises to accelerate healing and overcome longstanding challenges in bone defect repair. The study, led by Kui Huang from the Department of Oral and Maxillofacial Surgery at the Affiliated Stomatological Hospital of Southwest Medical University, introduces a multifunctional scaffold that not only enhances bone growth but also regulates immune responses and promotes vascularization.
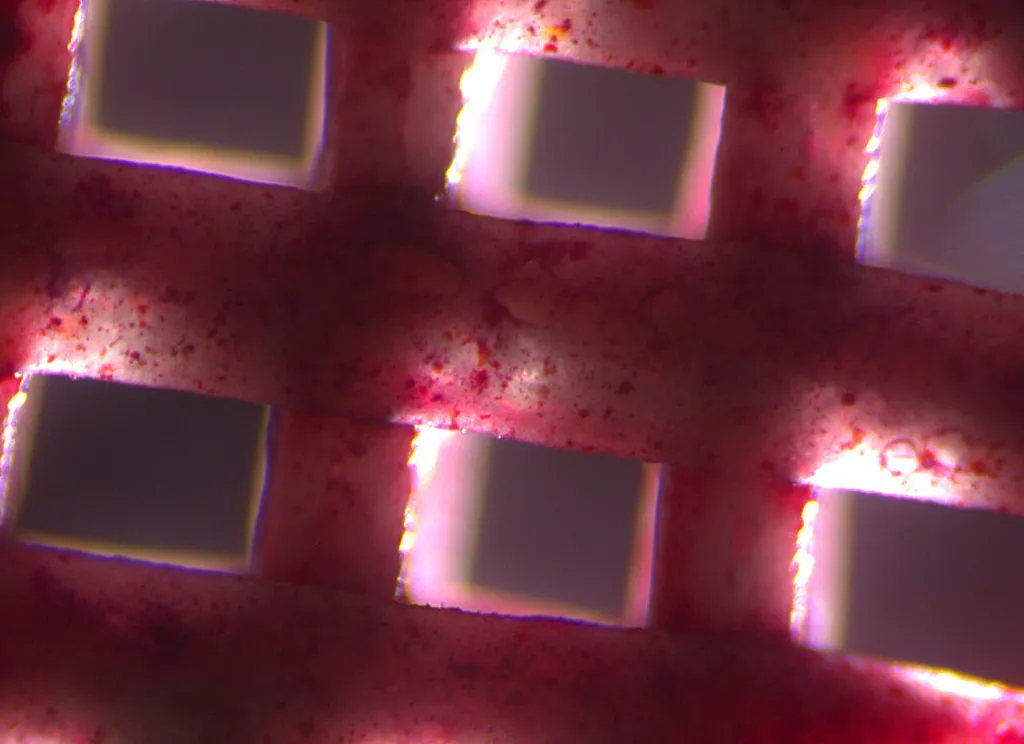
The EP@PCL/Sr scaffold, as it’s called, is a marvel of bioengineering. It combines a rough surface morphology that boosts cell proliferation and adhesion with a surface coating of epigallocatechin-3-gallate, a compound known for its immune-regulating properties. But the real innovation lies in the strontium-silk fibroin-modified hydroxyapatite embedded within the scaffold. This component releases strontium and calcium ions, which play a crucial role in both angiogenesis (the formation of new blood vessels) and osteogenesis (the formation of new bone).
“Our scaffold addresses two major hurdles in bone regeneration: the lack of vascularization and the risk of immune rejection,” Huang explained. “By integrating these multifunctional components, we’ve created a scaffold that not only promotes bone growth but also creates a favorable immune microenvironment and enhances vascularization.”
The results, published in the journal *Bioactive Materials* (translated as *活性材料* in Chinese), are promising. In both in vivo and ex vivo experiments, the EP@PCL/Sr scaffolds demonstrated excellent tissue compatibility, effective scavenging of reactive oxygen species, and strong regulation of the immune microenvironment. They also showed a remarkable ability to promote angiogenesis and osteogenesis, accelerating bone regeneration.
The implications for the medical field are substantial. Large bone defects, often resulting from trauma, tumors, or congenital conditions, have historically been difficult to treat. Current solutions often involve autografts or allografts, which come with their own set of challenges, including limited availability, donor site morbidity, and the risk of immune rejection. The EP@PCL/Sr scaffold offers a promising alternative, potentially reducing the need for such procedures and improving patient outcomes.
Moreover, the underlying mechanism revealed in the study—that the EP@PCL/Sr scaffolds promote osteogenesis of bone marrow stromal cells by activating the ITGA10/PI3K/AKT pathway—opens up new avenues for research and development in the field of bone tissue engineering.
As the world grapples with an aging population and an increasing prevalence of bone-related conditions, innovations like the EP@PCL/Sr scaffold are more important than ever. They not only hold the potential to improve patient care but also to drive economic growth in the medical device industry.
“This study presents a comprehensive and innovative strategy for bone regeneration and bone defect repair,” Huang said. “It provides a new possibility for clinical application and could shape the future of bone tissue engineering.”
Indeed, as researchers continue to refine and build upon this technology, the future of bone regeneration looks brighter than ever. The EP@PCL/Sr scaffold is not just a step forward; it’s a leap towards a future where bone defects can be repaired efficiently, effectively, and with minimal risk to the patient.