In the relentless battle against chronic wounds, particularly those stemming from diabetes, a groundbreaking study led by Tong Shen from the State Key Laboratory of Bioreactor Engineering at East China University of Science and Technology has unveiled a novel approach that harnesses the body’s own immune system to promote healing. The research, published in the journal *Bioactive Materials* (translated as *活性材料*), introduces a sophisticated biomaterial designed to modulate immune responses and mitigate chronic inflammation, offering a promising avenue for diabetic wound care.
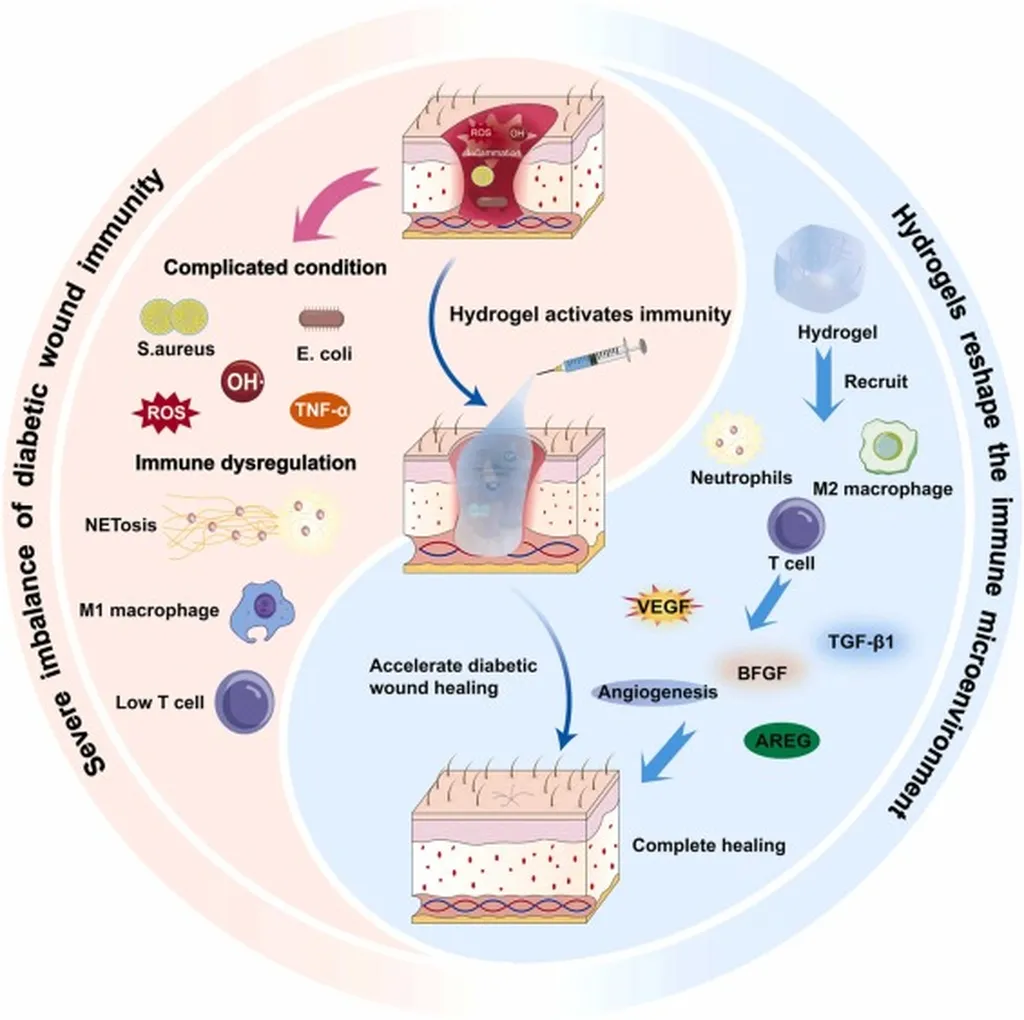
Diabetic wounds are notoriously difficult to treat due to persistent inflammation and immune dysregulation. Traditional treatments often fall short, leaving patients vulnerable to prolonged healing times and increased risk of complications. Shen and his team have developed a innovative solution by integrating sulfated chitosan (SCS), a chemically modified polysaccharide, with a microneedle structure to create an active immunomodulatory delivery system.
The key to this breakthrough lies in the sulfation domains of SCS, which enhance the material’s ability to bind cytokines and modulate immune responses. “The engineered sulfation domains confer synergistic cytokine-binding capacity to SCS, thereby equipping the material with enhanced functionality in immunomodulation,” explains Shen. This enhanced functionality drives macrophage polarization through the IL-4/STAT6-PPARγ cascade, triggering CCL22-dependent regulatory T cell (Treg) chemotaxis.
The result is a bidirectional crosstalk between macrophages and Tregs, creating a self-sustaining loop that resolves inflammation and promotes tissue repair. This biomaterial-driven coordination between innate and adaptive immunity represents a significant advancement over passive drug delivery approaches. “Our work pioneers endogenous immunity harnessing through biomaterial design, offering a paradigm shift for diabetic wound therapeutics,” says Shen.
The implications of this research extend beyond diabetic wound care, potentially impacting various sectors including the energy industry. Chronic wounds not only impose a significant burden on healthcare systems but also affect the quality of life for millions of patients. By providing a more effective and efficient treatment option, this innovative biomaterial could reduce healthcare costs and improve patient outcomes.
Moreover, the principles underlying this research could inspire new approaches to immune modulation in other chronic conditions, opening up avenues for further exploration and development. As the field of biomaterials continues to evolve, the integration of advanced technologies with biological systems holds immense promise for addressing some of the most pressing medical challenges of our time.
In the words of Shen, “This biomaterial-driven coordination between innate and adaptive immunity surpasses passive drug delivery approaches, effectively reducing inflammation and promoting wound healing without the need for exogenous biologics.” The study, published in *Bioactive Materials*, marks a significant step forward in the quest for more effective and targeted treatments for chronic wounds, offering hope to patients and healthcare providers alike.