In a groundbreaking development that could revolutionize the way we understand and treat atopic dermatitis (AD), a team of researchers led by Kyeong Seok Na from the Department of Bioengineering and Nano-Bioengineering at Incheon National University in South Korea has engineered novel hydrogel-based models that closely mimic the complex microenvironment of AD. This innovative research, published in the journal Bioactive Materials (which translates to “Active Biological Materials”), opens new avenues for preclinical drug screening and fundamental research into this chronic inflammatory condition.
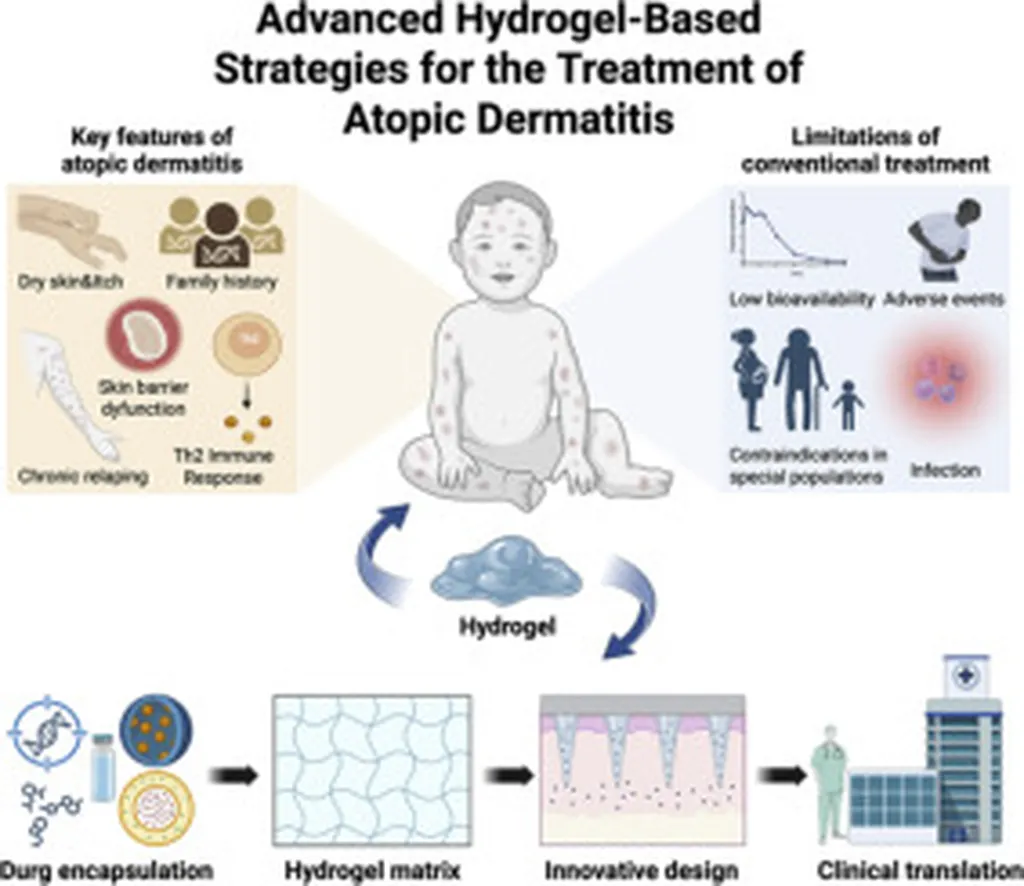
Atopic dermatitis, characterized by severe itching and inflammation, has long posed challenges due to its complex physiology and diverse pathogenesis. Traditional preclinical models have often fallen short in accurately replicating the nuances of AD, making it difficult to predict clinical outcomes. However, the team’s gelatin-based in situ crosslinkable hydrogel models are changing the game.
“We wanted to create a model that truly reflects the characteristics of AD tissue,” said Kyeong Seok Na, the lead author of the study. “By using single-cell RNA sequencing analysis, we confirmed key features such as the expression of collagen type VI alpha 5 chain (COL6A5+) fibroblasts, cell interactions with dorsal root ganglions that induce itching, and the overexpression of hypoxia-related factors in AD tissues.”
The researchers developed their artificial AD model by encapsulating cells within gelatin-based hydrogels, supporting 3D cell survival and growth. These models exhibit a hypoxic environment (pO2 < 5%) within the hydrogels, with upregulated expression of hypoxia-related genes. By treating the models with IL-4 and controlling oxygen concentration, the team successfully recreated the AD microenvironment, inducing immune responses and chronic hypoxia. "This platform allows us to evaluate drug responses under conditions that closely mimic those in actual AD patients," Na explained. "We can analyze the overexpression of itch-related factors and gene upregulation under hypoxic and immune conditions, providing valuable insights for drug development." The implications of this research are profound. By offering a more accurate and reliable preclinical model, the team's work could significantly accelerate the development of new treatments for atopic dermatitis. This could lead to improved patient outcomes and a better understanding of the underlying mechanisms of the disease. Moreover, the innovative use of polymeric hydrogels in engineered skin tissue models highlights the potential for these materials in other areas of biomedical research. The ability to recreate complex microenvironments could pave the way for advancements in tissue engineering, regenerative medicine, and drug discovery. As the field continues to evolve, the work of Kyeong Seok Na and his team serves as a testament to the power of interdisciplinary research. By combining bioengineering, nanotechnology, and advanced analytical techniques, they have made a significant stride towards unraveling the complexities of atopic dermatitis and improving patient care. In the broader context, this research underscores the importance of developing sophisticated models that can faithfully replicate the intricacies of human diseases. As we move forward, such models will be instrumental in bridging the gap between preclinical research and clinical application, ultimately benefiting patients and advancing the field of medicine.