In a significant stride towards enhancing patient care and preventing pressure ulcers, researchers at the Querrey Simpson Institute for Bioelectronics at Northwestern University have developed a groundbreaking wireless, skin-integrated system for continuous pressure distribution monitoring. This innovative technology, led by Seonggwang Yoo, promises to revolutionize healthcare environments by providing real-time data that can prevent ischemic damage, infections, and prolonged hospital stays.
Pressure ulcers, a persistent challenge in healthcare, particularly affect individuals with limited mobility or compromised sensation. Early detection is crucial, yet conventional sensing technologies integrated into mattresses have limitations. They are restricted to stationary environments and often miss critical data when patients move or change positions. Moreover, these systems lack the ability to provide consistent information on the specific spatial distribution of pressure across the body.
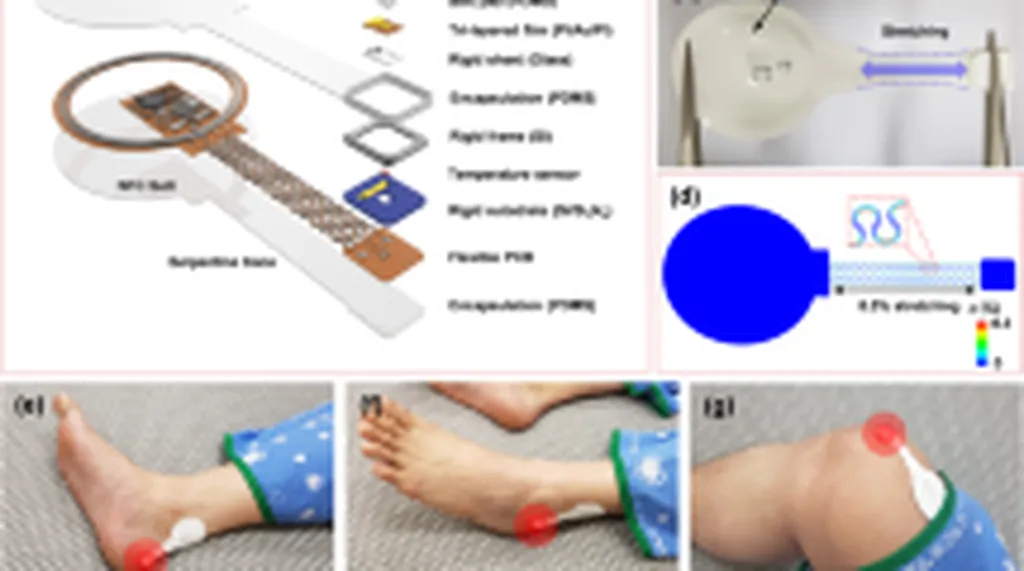
The new system, detailed in a study published in ‘npj Flexible Electronics’ (which translates to ‘npj Flexible Electronics’ in English), addresses these shortcomings with a design that mounts directly on the skin. “Our system features an array of soft, elastomer-encapsulated pressure sensors that minimize discomfort,” explains Yoo. “It operates wirelessly, with an independent power management system, making it versatile for use in homes, outpatient facilities, and operating rooms.”
One of the standout features of this technology is its ability to deliver immediate feedback. An external alarm satellite device provides vibratory and visual alerts if predefined pressure thresholds are exceeded, guiding caregivers or patients to take timely action. “This real-time feedback is a game-changer,” Yoo notes. “It empowers patients and caregivers to make informed decisions quickly, potentially preventing serious complications.”
The system’s design principles are supported by both experimental and finite element analysis, ensuring its reliability and effectiveness. Deployments on patients in hospital settings have already illustrated practical use cases, demonstrating the system’s potential to transform patient care.
The implications of this research extend beyond immediate healthcare applications. The technology’s ability to provide continuous, accurate data could lead to advancements in personalized medicine, where treatment plans are tailored based on real-time patient data. Additionally, the system’s wireless and wearable nature opens doors for integration with other health monitoring technologies, creating a comprehensive ecosystem for patient care.
As the healthcare industry continues to evolve, the demand for innovative, patient-centric technologies will only grow. This research by Yoo and his team at the Querrey Simpson Institute for Bioelectronics at Northwestern University sets a new standard for pressure monitoring systems, paving the way for future developments in wearable health technologies. The study’s publication in ‘npj Flexible Electronics’ underscores its significance and potential impact on the field.
In the broader context, this technology could also influence the energy sector by driving demand for advanced materials and manufacturing processes that support the production of flexible, wearable electronics. As the healthcare industry adopts more sophisticated monitoring systems, the energy sector will need to innovate to meet the power requirements of these devices, potentially leading to advancements in energy storage and wireless power transmission technologies.
The research not only highlights the importance of early detection and prevention in healthcare but also showcases the potential of interdisciplinary collaboration in driving technological innovation. By combining expertise in bioelectronics, materials science, and healthcare, Yoo and his team have created a system that has the potential to significantly improve patient outcomes and transform the way healthcare is delivered.